Avian influenza
| Influenza (flu) |
|---|
 |
Avian influenza, also known as avian flu or bird flu, is a disease caused by the influenza A virus, which primarily affects birds but can sometimes affect mammals including humans.[1] Wild aquatic birds are the primary host of the influenza A virus, which is enzootic (continually present) in many bird populations.[2][3]
Symptoms of avian influenza vary according to both the strain of virus underlying the infection, and on the species of bird or mammal affected. Classification of a virus strain as either low pathogenic avian influenza (LPAI) or high pathogenic avian influenza (HPAI) is based on the severity of symptoms in domestic chickens and does not predict severity of symptoms in other species.[4] Chickens infected with LPAI display mild symptoms or are asymptomatic, whereas HPAI causes serious breathing difficulties, significant drop in egg production, and sudden death.[5] Domestic poultry may potentially be protected from specific strains of the virus by vaccination.[6]
Humans and other mammals can only become infected with avian influenza after prolonged close contact with infected birds.[7] In mammals including humans, infection with avian influenza (whether LPAI or HPAI) is rare. Symptoms of infection vary from mild to severe, including fever, diarrhea, and cough.[8]
Influenza A virus is shed in the saliva, mucus, and feces of infected birds; other infected animals may shed bird flu viruses in respiratory secretions and other body fluids (e.g., cow milk).[9] The virus can spread rapidly through poultry flocks and among wild birds.[9] A particularly virulent strain, influenza A virus subtype H5N1 (A/H5N1) has the potential to decimate domesticated poultry stocks and an estimated half a billion farmed birds have been slaughtered in efforts to contain the virus.[10]
Highly pathogenic avian influenza
[edit]Because of the impact of avian influenza on economically important chicken farms, a classification system was devised in 1981 which divided avian virus strains as either highly pathogenic (and therefore potentially requiring vigorous control measures) or low pathogenic. The test for this is based solely on the effect on chickens - a virus strain is highly pathogenic avian influenza (HPAI) if 75% or more of chickens die after being deliberately infected with it. The alternative classification is low pathogenic avian influenza (LPAI).[11] This classification system has since been modified to take into account the structure of the virus' haemagglutinin protein.[12] Other species of birds, especially water birds, can become infected with HPAI virus without experiencing severe symptoms and can spread the infection over large distances; the exact symptoms depend on the species of bird and the strain of virus.[11] Classification of an avian virus strain as HPAI or LPAI does not predict how serious the disease might be if it infects humans or other mammals.[11][13]
Since 2006, the World Organization for Animal Health requires all LPAI H5 and H7 detections to be reported because of their potential to mutate into highly pathogenic strains.[14]
Virology
[edit]
Avian influenza is caused by the influenza A virus which principally affects birds but can also infect humans and other mammals.[16][17] Influenza A is an RNA virus with a genome comprising a negative-sense, RNA segmented genome that encodes for 11 viral genes.[18] The virus particle (also called the virion) is 80–120 nanometers in diameter and elliptical or filamentous in shape.[19][20] There is evidence that the virus can survive for long periods in freshwater after being excreted in feces by its avian host, and can withstand prolonged freezing.[21]
There are two proteins on the surface of the viral envelope; hemagglutinin and neuraminidase.[4] These are the major antigens of the virus against which neutralizing antibodies are produced. Influenza virus epidemics and epizootics are associated with changes in their antigenic structure.[22]
Hemagglutinin (H) is an antigenic glycoprotein which allows the virus to bind to and enter the host cell. Neuraminidase (N) is an antigenic glycosylated enzyme which facilitates the release of progeny viruses from infected cells.[23] There are 18 known types of hemagglutinin, of which H1 thru H16 have been found in birds, and 11 types of neuraminidase.[16]
Subtypes
[edit]Subtypes of influenza A are defined by the combination of H and N proteins in the viral envelope; for example, "H5N1" designates an influenza A subtype that has a type-5 hemagglutinin (H) protein and a type-1 neuraminidase (N) protein.[7] The subtyping scheme only takes into account the two envelope proteins, not the other proteins coded by the virus' RNA. Almost all possible combinations of H (1 thru 16) and N (1 thru 11) have been isolated from wild birds.[24] Further variations exist within the subtypes and can lead to very significant differences in the virus's ability to infect and cause disease.[25]
Influenza virus nomenclature
[edit]
To unambiguously describe a specific isolate of virus, researchers use the internationally accepted Influenza virus nomenclature,[26] which describes, among other things, the species of animal from which the virus was isolated, and the place and year of collection. As an example - A/chicken/Nakorn-Patom/Thailand/CU-K2/04(H5N1):
- A stands for the genus of influenza (A, B or C).
- chicken is the animal species the isolate was found in (note: human isolates lack this component term and are thus identified as human isolates by default)
- Nakorn-Patom/Thailand is the place this specific virus was isolated
- CU-K2 is the laboratory reference number that identifies it from other influenza viruses isolated at the same place and year
- 04 represents the year of isolation 2004
- H5 stands for the fifth of several known types of the protein hemagglutinin.
- N1 stands for the first of several known types of the protein neuraminidase.
Other examples include: A/duck/Hong Kong/308/78(H5N3), A/avian/NY/01(H5N2), A/chicken/Mexico/31381-3/94(H5N2), and A/shoveler/Egypt/03(H5N2).[27]
Genetic characterization
[edit]Analysis of the virus' genome enables researchers to determine the order of its nucleotides. Comparison of the genome of a virus with that of a different virus can reveal differences between the two viruses.[16][28] Genetic variations are important because they can change amino acids that make up the influenza virus’ proteins, resulting in structural changes to the proteins, and thereby altering properties of the virus. Some of these properties include the ability to evade immunity and the ability to cause severe disease.[28]
Genetic sequencing enables influenza strains to be further characterised by their clade or subclade, revealing links between different samples of virus and tracing the evolution of the virus over time.[28]
Species barrier
[edit]Rarely, humans can become infected by the avian flu if they are in close contact with infected birds. Symptoms vary from mild to severe (including death), but these instances have not sustained transmission from one person to another.[4][17]
There are a number of factors that generally prevent the avian flu from causing epidemics in humans or other mammals.[29][30] One of them is that the HA protein of avian influenza binds to alpha-2,3 sialic acid receptors, which are present in the respiratory tract and intestines of avian species, while human influenza HA binds to alpha-2,6 sialic acid receptors, which are present in the human upper respiratory tract.[31][32] Other factors include the ability to replicate the viral RNA genome within the host cell nucleus, to evade host immune responses, and to transmit between individuals.[33]
Influenza viruses are constantly changing as small genetic mutations accumulate, a process known as antigenic drift. Over time, mutation may lead to a change in antigenic properties such that host antibodies (acquired through vaccination or prior infection) do not provide effective protection, causing a fresh outbreak of disease.[34]
The segmented genome of influenza viruses facilitates genetic reassortment. This can occur if a host is infected simultaneously with two different strains of influenza virus; then it is possible for the viruses to interchange genetic material as they reproduce in the host cells.[35] Thus, an avian influenza virus can acquire characteristics, such as the ability to infect humans, from a different virus strain. The presence of both alpha 2,3 and alpha 2,6 sialic acid receptors in pig tissues allows for co-infection by avian influenza and human influenza viruses. This susceptibility makes pigs a potential "melting pot" for the reassortment of influenza A viruses.[36]
Epidemiology
[edit]History
[edit]Avian influenza (historically known as fowl plague) is caused by bird-adapted strains of the influenza type A virus.[4] The disease was first identified by Edoardo Perroncito in 1878 when it was differentiated from other diseases that caused high mortality rates in birds; in 1955 it was established that the fowl plague virus was closely related to human influenza. In 1972 it became evident that many subtypes of avian flu were endemic in wild bird populations.[11]
Between 1959 and 1995, there were 15 recorded outbreaks of highly pathogenic avian influenza (HPAI) in poultry, with losses varying from a few birds on a single farm to many millions. Between 1996 and 2008, HPAI outbreaks in poultry have been recorded at least 11 times and 4 of these outbreaks have resulted in the death or culling of millions of birds.[11] Since then, several virus strains (both LPAI and HPAI) have become endemic among wild birds with increasingly frequent outbreaks among domestic poultry, especially of the H5 and H7 subtypes.
Transmission and prevention
[edit]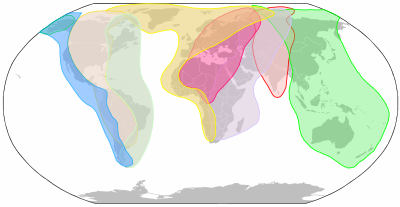
Birds - Influenza A viruses of various subtypes have a large reservoir in wild waterbirds of the orders Anseriformes (for example, ducks, geese, and swans) and Charadriiformes (for example, gulls, terns, and waders) which can infect the respiratory and gastrointestinal tract without affecting the health of the host.[38] They can then be carried by the bird over large distances, especially during annual migration. Infected birds can shed avian influenza A viruses in their saliva, nasal secretions, and feces; susceptible birds become infected when they have contact with the virus as it is shed by infected birds.[39] The virus can survive for long periods in water and at low temperatures, and can be spread from one farm to another on farm equipment.[40] Domesticated birds (chickens, turkeys, ducks, etc.) may become infected with avian influenza A viruses through direct contact with infected waterfowl or other infected poultry, or through contact with contaminated feces or surfaces.
Avian influenza outbreaks in domesticated birds are of concern for several reasons. There is potential for low pathogenic avian influenza viruses (LPAI) to evolve into strains which are high pathogenic to poultry (HPAI), and subsequent potential for significant illness and death among poultry during outbreaks. Because of this, international regulations state that any detection of H5 or H7 subtypes (regardless of their pathogenicity) must be notified to the appropriate authority.[41][42] It is also possible that avian influenza viruses could be transmitted to humans and other animals which have been exposed to infected birds, causing infection with unpredictable but sometimes fatal consequences.
When an HPAI infection is detected in poultry, it is normal to cull infected animals and those nearby in an effort to rapidly contain, control and eradicate the disease. This is done together with movement restrictions, improved hygiene and biosecurity, and enhanced surveillance. [40]
Humans - Avian flu viruses, both HPAI and LPAI, can infect humans who are in close, unprotected contact with infected poultry. Incidents of cross-species transmission are rare, with symptoms ranging in severity from no symptoms or mild illness, to severe disease that resulted in death.[43][42] As of February, 2024 there have been very few instances of human-to-human transmission, and each outbreak has been limited to a few people.[44] All subtypes of avian Influenza A have potential to cross the species barrier, with H5N1 and H7N9 considered the biggest threats.[45][46]
In order to avoid infection, the general public are advised to avoid contact with sick birds or potentially contaminated material such as carcasses or feces. People working with birds, such as conservationists or poultry workers, are advised to wear appropriate personal protection equipment.[47]
Other animals - a wide range of other animals have been affected by avian flu, generally due to eating birds which had been infected.[48] There have been instances where transmission of the disease between mammals, including seals and cows, may have occurred.[49][50]
Pandemic potential
[edit]Influenza viruses have a relatively high mutation rate that is characteristic of RNA viruses.[51] The segmentation of the influenza A virus genome facilitates genetic recombination by segment reassortment in hosts who become infected with two different strains of influenza viruses at the same time.[52][53] With reassortment between strains, an avian strain which does not affect humans may acquire characteristics from a different strain which enable it to infect and pass between humans - a zoonotic event.[39] It is thought that all influenza A viruses causing outbreaks or pandemics among humans since the 1900s originated from strains circulating in wild aquatic birds through reassortment with other influenza strains.[54][55] It is possible (though not certain) that pigs may act as an intermediate host for reassortment.[56]
As of June 2024, there is concern about two subtypes of avian influenza which are circulating in wild bird populations worldwide, H5N1 and H7N9. Both of these have potential to devastate poultry stocks, and both have jumped to humans with relatively high case fatality rates.[57]
Surveillance
[edit]The Global Influenza Surveillance and Response System (GISRS) is a global network of laboratories that monitor the spread of influenza with the aim to provide the World Health Organization with influenza control information and to inform vaccine development.[58] Several millions of specimens are tested by the GISRS network annually through a network of laboratories in 127 countries.[59] As well as human viruses, GISRS monitors avian, swine, and other potentially zoonotic influenza viruses.
Vaccine
[edit]Poultry - it is possible to vaccinate poultry against specific strains of HPAI influenza. Vaccination should be combined with other control measures such as infection monitoring, early detection and biosecurity.[60][61]
Humans - Several "candidate vaccines" are available in case of an avian virus acquires the ability to infect and transmit among humans. There are strategic stockpiles of vaccines against the H5N1 subtype which is considered the biggest risk.[62][63][64] A vaccine against the H7N9 subtype, which has also infected humans, has undergone a limited amount of testing.[65] In the event of an outbreak, the "candidate" vaccine would be rapidly tested for safety as well as efficacy against the zoonotic strain, and then authorised and distributed to vaccine manufacturers.[66]
Zoonotic influenza vaccine Seqirus is authorized for use in the European Union.[67] It is an H5N8 vaccine that is intended to provide acquired immunity against H5 subtype influenza A viruses.[67]
Influenza A virus subtype H5N1
[edit] |
The highly pathogenic influenza A virus subtype H5N1 is an emerging avian influenza virus that is causing global concern as a potential pandemic threat. It is often referred to simply as "bird flu" or "avian influenza", even though it is only one of many subtypes.
A/H5N1 has killed millions of poultry in a growing number of countries throughout Asia, Europe, and Africa. Health experts are concerned that the coexistence of human flu viruses and avian flu viruses (especially H5N1) will provide an opportunity for genetic material to be exchanged between species-specific viruses, possibly creating a new virulent influenza strain that is easily transmissible and lethal to humans.[68]
Influenza A/H5N1 was first recorded in a small outbreak among poultry in Scotland[69] in 1959, with numerous outbreaks subsequently in every continent.[70] The first known transmission of A/H5N1 to a human occurred in Hong Kong in 1997, when there was an outbreak of 18 human cases resulting in 6 deaths. It was determined that all the infected people had been exposed to infected birds in poultry markets. As the disease continued to spread among poultry flocks in the territory, the decision was made to cull all 1.6 million poultry in the area and to impose strict controls on the movement and handling of poultry.This terminated the outbreak.[71][72]
There is weak evidence to support limited human-to-human transmission of A/H5N1 in 139 outreaks between 2005 and 2009 in Sumatra. The reproduction number was well below the threshold for sustained transmission.[73]
Between 2003 and November 2024, the World Health Organization has recorded 948 cases of confirmed H5N1 influenza, leading to 464 deaths.[74] The true fatality rate may be lower because some cases with mild symptoms may not have been identified as H5N1.[75]
Influenza A virus subtype H7N9
[edit]
A significant outbreak of influenza A virus subtype H7N9 (A/H7N9) started in March 2013 when severe influenza affected 18 humans in China; six subsequently died.[76] It was discovered that a low pathogenic strain of A/H7N9 was circulating among chickens, and that all the affected people had been exposed in poultry markets. Further cases among humans and poultry in mainland China continued to be identified sporadically throughout the year, followed by a peak around the festival season of Chinese New Year (January and February) in early 2014 which was attributed to the seasonal surge in poultry production. Up to December 2013, there had been 139 cases with 47 deaths.[77]
Infections among humans and poultry continued during the next few years, again with peaks around the new year. In 2016 a virus strain emerged which was highly pathogenic to chickens.[78][79] In order to contain the HPAI outbreak, the Chinese authorities in 2017 initiated a large scale vaccination campaign against avian influenza in poultry. Since then, the number of outbreaks in poultry, as well as the number of human cases, dropped significantly. In humans, symptoms and mortality for both LPAI and HPAI strains have been similar.[78] Although no human H7N9 infections have been reported since February 2019, the virus is still circulating in poultry, particularly in laying hens. It has demonstrated antigenic drift to evade vaccines, and remains a potential threat to the poultry industry and public health.[79]
Genetic and evolutionary analyses have shown that the A(H7) viruses in the Chinese outbreak probably transferred from domestic duck to chicken populations in China and then reassorted with poultry influenza A(H9N2) to generate the influenza A(H7N9) strain that affected humans. The genetic characteristics of A(H7N9) virus are of concern because of their pandemic potential, e.g. their potential to recognise human and avian influenza virus receptors which affects the ability to cause sustained human-to-human transmission, or the ability to replicate in the human host.[76]
Between February 2013 and February 2019 there were 1,568 confirmed human cases and 616 deaths associated with the outbreak in China.[80][81] The majority of human cases have reported contact with poultry in markets or farms. Transmission between humans remains limited with some evidence of small family clusters. However, there is no evidence of sustained human-to-human transmission of A/H7N9 influenza.[78]
During early 2017, outbreaks of avian influenza A(H7N9) occurred in poultry in the USA. The strain in these outbreaks was of North American origin and is unrelated to the Asian lineage H7N9 which is associated with human infections in China.[78]
Domestic animals
[edit]
Several domestic species have been infected with and shown symptoms of H5N1 viral infection, including cats, dogs, ferrets, pigs, and birds.[82]
Poultry
[edit]Attempts are made in the United States to minimize the presence of HPAI in poultry through routine surveillance of poultry flocks in commercial poultry operations. Detection of a HPAI virus may result in immediate culling of the flock. Less pathogenic viruses are controlled by vaccination.[83]
Dairy cows
[edit]During April 2024 avian influenza was first detected in dairy cows in several US states and subsequently spread more widely through the year. Influenza A(H5N1) was found to be present at high levels in the mammary glands and in the milk of affected cows.[84][85][86] It was shown that the virus can persist on milking equipment, which provides a probable transmission route for cow-to-cow and cow-to-human spread.[87] A number of humans who had been in contact with cows tested positive for the virus, with mild symptoms.[88] According to CDC 7 % of 115 dairy workers had evidence of recent infection in a study from Michigan and Colorado from June to August 2024- half of them asymptomatic. This is higher than estimates from prior transmission studies in poultry. All dairy workers had worked in cleaning the milk parlor and none had used personal protective equipment.[89]
Cats
[edit]Global aspects
[edit]Global measures
[edit]In 2005, the formation of the International Partnership on Avian and Pandemic Influenza was announced in order to elevate the importance of avian flu, coordinate efforts, and improve disease reporting and surveillance in order to better respond to future pandemics. New networks of laboratories have emerged to detect and respond to avian flu, such as the Crisis Management Center for Animal Health, the Global Avian Influenza Network for Surveillance, OFFLU, and the Global Early Warning System for major animal diseases. After the 2003 outbreak, WHO member states have also recognized the need for more transparent and equitable sharing of vaccines and other benefits from these networks.[93] Cooperative measures created in response to HPAI have served as a basis for programs related to other emerging and re-emerging infectious diseases.
Impact on national policies
[edit]HPAI control has also been used for political ends. In Indonesia, negotiations with global response networks were used to recentralize power and funding to the Ministry of Health.[94] In Vietnam policymakers, with the support of the Food and Agriculture Organization of the United Nations (FAO), used HPAI control to accelerate the industrialization of livestock production for export by proposing to increase the portion of large-scale commercial farms and reducing the number of poultry keepers from 8 to 2 million by 2010.[95]
Traditional Asian practices
[edit]Backyard poultry production was viewed as "traditional Asian" agricultural practices that contrasted with modern commercial poultry production and seen as a threat to biosecurity. Backyard production appeared to hold greater risk than commercial production due to lack of biosecurity and close contact with humans, though HPAI spread in intensively raised flocks was greater due to high density rearing and genetic homogeneity.[96][97] Asian culture itself was blamed as the reason why certain interventions, such as those that only looked at placed-based interventions, would fail without looking for multifaceted solutions.[95]
Economic impact
[edit]Approximately 20% of the protein consumed in developing countries come from poultry.[96] A report by FAO totalled economic losses caused by avian influenza in South East Asia up to 2005 around US$10 billion. This had the greatest impact on small scale commercial and backyard producers.[98]
As poultry serves as a source of food security and liquid assets, the most vulnerable populations were poor small scale farmers.[95] The loss of birds due to HPAI and culling in Vietnam led to an average loss of 2.3 months of production and US$69–108 for households where many have an income of $2 a day or less.[98] The loss of food security for vulnerable households can be seen in the stunting of children under five in Egypt. Women are another population at risk as in most regions of the world, small flocks are tended to by women. Widespread culling also resulted in the decreased enrollment of girls in school in Turkey.[96]
See also
[edit]- Global spread of H5N1
- Subtypes of Influenza A virus
- Influenza A virus subtype H5N1
- Influenza A virus subtype H7N9
- Influenza
- Influenza A virus
- Influenza pandemic
- Influenza Genome Sequencing Project
- Influenza research
- Influenza vaccine
- International Partnership on Avian and Pandemic Influenza
- OIE/FAO Network of Expertise on Animal Influenza
Notes
[edit]References
[edit]- ^ "Avian Influenza A H5N1 - United Kingdom of Great Britain and Northern Ireland". www.who.int. Retrieved 2024-05-16.
- ^ Li YT, Linster M, Mendenhall IH, Su YC, Smith GJ (December 2019). "Avian influenza viruses in humans: lessons from past outbreaks". British Medical Bulletin. 132 (1): 81–95. doi:10.1093/bmb/ldz036. PMC 6992886. PMID 31848585.
- ^ Joseph U, Su YC, Vijaykrishna D, Smith GJ (January 2017). "The ecology and adaptive evolution of influenza A interspecies transmission". Influenza and Other Respiratory Viruses. 11 (1): 74–84. doi:10.1111/irv.12412. PMC 5155642. PMID 27426214.
- ^ a b c d "Avian Influenza in Birds". U.S. Centers for Disease Control and Prevention (CDC). 2022-06-14. Retrieved 2024-05-06.
- ^ "Bird flu (avian influenza): how to spot and report it in poultry or other captive birds". Department for Environment, Food & Rural Affairs and Animal and Plant Health Agency. 2022-12-13. Retrieved 2024-05-06.
- ^ "Vaccination of poultry against highly pathogenic avian influenza – Available vaccines and vaccination strategies". www.efsa.europa.eu. 2023-10-10. Retrieved 2024-05-09.
- ^ a b "Influenza Type A Viruses". U.S. Centers for Disease Control and Prevention (CDC). 2024-02-01. Retrieved 2024-05-03.
- ^ "Avian influenza: guidance, data and analysis". GOV.UK. 2021-11-18. Retrieved 2024-05-09.
- ^ a b "Prevention and Antiviral Treatment of Bird Flu Viruses in People". Centers for Disease Control. 2024-04-19.
- ^ Bourk I (26 April 2024). "'Unprecedented': How bird flu became an animal pandemic". www.bbc.com. Retrieved 2024-05-08.
- ^ a b c d e Alexander DJ, Brown IH (April 2009). "History of highly pathogenic avian influenza". Revue Scientifique et Technique. 28 (1): 19–38. doi:10.20506/rst.28.1.1856. PMID 19618616.
- ^ "Factsheet on A(H5N1)". www.ecdc.europa.eu. 2017-06-15. Retrieved 2024-05-21.
- ^ "Current U.S. Bird Flu Situation in Humans". U.S. Centers for Disease Control and Prevention (CDC). 2024-04-05. Retrieved 2024-05-22.
- ^ "National H5/H7 Avian Influenza surveillance plan". United States Department of Agriculture. Animal Plant Health Inspection Service. October 2013.
- ^ "Recreated 1918 Influenza virions". U.S. Centers for Disease Control and Prevention (CDC). Archived from the original on 26 October 2020. Retrieved 24 April 2018.
- ^ a b c "Types of Influenza Viruses". U.S. Centers for Disease Control and Prevention (CDC). 2023-03-30. Retrieved 2024-05-22.
- ^ a b "Influenza (Avian and other zoonotic)". World Health Organization. 3 October 2023. Retrieved 2024-05-06.
- ^ Samji T (December 2009). "Influenza A: understanding the viral life cycle". The Yale Journal of Biology and Medicine. 82 (4): 153–159. PMC 2794490. PMID 20027280.
- ^ Noda T (2011). "Native morphology of influenza virions". Frontiers in Microbiology. 2: 269. doi:10.3389/fmicb.2011.00269. PMC 3249889. PMID 22291683.
- ^ Dadonaite B, Vijayakrishnan S, Fodor E, Bhella D, Hutchinson EC (August 2016). "Filamentous influenza viruses". The Journal of General Virology. 97 (8): 1755–1764. doi:10.1099/jgv.0.000535. PMC 5935222. PMID 27365089.
- ^ Shoham D, Jahangir A, Ruenphet S, Takehara K (2012-10-04). "Persistence of avian influenza viruses in various artificially frozen environmental water types". Influenza Research and Treatment. 2012: 912326. doi:10.1155/2012/912326. PMC 3471417. PMID 23091712.
- ^ "Avian Influenza". NIOSH Workplace Safety and Health Topic. National Institute for Occupational Safety and Health. 2018-10-17.
- ^ Couch R (1996). "Chapter 58. Orthomyxoviruses Multiplication". In Baron S (ed.). Medical Microbiology. Galveston: The University of Texas Medical Branch at Galveston. ISBN 978-0-9631172-1-2. PMID 21413353. Archived from the original on May 3, 2009.
- ^ "FluGlobalNet - Avian Influenza". science.vla.gov.uk. Retrieved 2024-06-05.
- ^ Eisfeld AJ, Neumann G, Kawaoka Y (January 2015). "At the centre: influenza A virus ribonucleoproteins". Nature Reviews. Microbiology. 13 (1): 28–41. doi:10.1038/nrmicro3367. PMC 5619696. PMID 25417656.
- ^ "A revision of the system of nomenclature for influenza viruses: a WHO memorandum". Bulletin of the World Health Organization. 58 (4): 585–591. 1980. PMC 2395936. PMID 6969132.
This Memorandum was drafted by the signatories listed on page 590 on the occasion of a meeting held in Geneva in February 1980.
- ^ Payungporn S, Chutinimitkul S, Chaisingh A, Damrongwantanapokin S, Nuansrichay B, Pinyochon W, et al. (April 2006). "Discrimination between highly pathogenic and low pathogenic H5 avian influenza A viruses". Emerging Infectious Diseases. 12 (4): 700–701. doi:10.3201/eid1204.051427. PMC 3294708. PMID 16715581.
- ^ a b c "Influenza Virus Genome Sequencing and Genetic Characterization". Centers for Disease Control and Prevention. 2024-02-27. Retrieved 2024-05-24.
- ^ Petric PP, Schwemmle M, Graf L (July 2023). "Anti-influenza A virus restriction factors that shape the human species barrier and virus evolution". PLOS Pathogens. 19 (7): e1011450. doi:10.1371/journal.ppat.1011450. PMC 10325056. PMID 37410755.
- ^ Koçer ZA, Jones JC, Webster RG (December 2013). Atlas RM, Maloy S (eds.). "Emergence of Influenza Viruses and Crossing the Species Barrier". Microbiology Spectrum. 1 (2). doi:10.1128/microbiolspec.OH-0010-2012. PMID 26184958.
- ^ Bertram S, Glowacka I, Steffen I, Kühl A, Pöhlmann S (September 2010). "Novel insights into proteolytic cleavage of influenza virus hemagglutinin". Reviews in Medical Virology. 20 (5): 298–310. doi:10.1002/rmv.657. PMC 7169116. PMID 20629046.
The influenza virus HA binds to alpha 2–3 linked (avian viruses) or alpha 2–6 linked (human viruses) sialic acids presented by proteins or lipids on the host cell surface.
- ^ Kuchipudi SV, Nelli RK, Gontu A, Satyakumar R, Surendran Nair M, Subbiah M (February 2021). "Sialic Acid Receptors: The Key to Solving the Enigma of Zoonotic Virus Spillover". Viruses. 13 (2): 262. doi:10.3390/v13020262. PMC 7915228. PMID 33567791.
- ^ Long JS, Mistry B, Haslam SM, Barclay WS (January 2019). "Host and viral determinants of influenza A virus species specificity". Nature Reviews. Microbiology. 17 (2): 67–81. doi:10.1038/s41579-018-0115-z. PMID 30487536.
- ^ "How Flu Viruses Can Change". U.S. Centers for Disease Control and Prevention (CDC). 2022-12-12. Retrieved 2024-05-22.
- ^ Steel J, Lowen AC (2014), Compans RW, Oldstone MB (eds.), "Influenza a Virus Reassortment", Influenza Pathogenesis and Control - Volume I, Current Topics in Microbiology and Immunology, vol. 385, Cham: Springer International Publishing, pp. 377–401, doi:10.1007/82_2014_395, ISBN 978-3-319-11155-1, PMID 25007845
- ^ Schnitzler SU, Schnitzler P (December 2009). "An update on swine-origin influenza virus A/H1N1: a review". Virus Genes. 39 (3): 279–292. doi:10.1007/s11262-009-0404-8. PMC 7088521. PMID 19809872.
If an avian virus mutates or reassorts and gains the ability to bind to α2,6 linked sialic acids, it might cross the species barrier and infect humans. Swine tissues express both forms of sialic acid and can be coinfected with human and avian viruses. Thus, pigs serve as a melting vessel for human, avian and swine influenza strains.
- ^ Thompson D, Byrkjedal I (2001). Shorebirds. Colin Baxter Photography Ltd. ISBN 978-1841070759.
- ^ "Mitigation strategy for avian influenza in wild birds in England and Wales". GOV.UK - Department for Environment Food & Rural Affairs. 18 March 2024. Retrieved 2024-07-25.
- ^ a b "Transmission of Bird Flu Viruses Between Animals and People". U.S. Centers for Disease Control and Prevention (CDC). 2024-05-15. Retrieved 2024-06-10.
- ^ a b "Avian Influenza". WOAH - World Organisation for Animal Health. Retrieved 2024-06-10.
- ^ "Prevention and Control of H5 and H7 Avian Influenza in the Live Bird Marketing System". United States Department of Agriculture. August 2020. Retrieved 15 June 2024.
- ^ a b "Questions and Answers on Avian Influenza". An official website of the European Commission. 11 June 2024. Retrieved 2024-06-11.
- ^ "Avian Influenza A Virus Infections in Humans". U.S. Centers for Disease Control and Prevention (CDC). 2024-05-30. Retrieved 2024-06-11.
- ^ "Reported Human Infections with Avian Influenza A Viruses". Centers for Disease Control and Prevention. 2024-02-01. Retrieved 2024-06-11.
- ^ "Zoonotic influenza". Wordl Health Organization. Retrieved 2024-06-16.
- ^ "The next pandemic: H5N1 and H7N9 influenza?". Gavi, the Vaccine Alliance. Retrieved 2024-06-16.
- ^ "Highly Pathogenic Avian Influenza A(H5N1) Virus in Animals: Interim Recommendations for Prevention, Monitoring, and Public Health Investigations". U.S. Centers for Disease Control and Prevention. 2024-06-05. Retrieved 2024-06-13.
- ^ "Bird flu 'spills over' to otters and foxes in UK". BBC News. 2023-02-02. Retrieved 2024-06-11.
- ^ "Study of H5N1 avian flu seal deaths reveals multiple lineages". Center for Infectious Disease Research and Policy. 2023-03-15. Retrieved 2024-06-13.
- ^ Kozlov M (June 2024). "Huge amounts of bird-flu virus found in raw milk of infected cows". Nature. doi:10.1038/d41586-024-01624-1. PMID 38840011.
- ^ Sanjuán R, Nebot MR, Chirico N, Mansky LM, Belshaw R (October 2010). "Viral mutation rates". Journal of Virology. 84 (19): 9733–9748. doi:10.1128/JVI.00694-10. PMC 2937809. PMID 20660197.
- ^ Kou Z, Lei FM, Yu J, Fan ZJ, Yin ZH, Jia CX, et al. (December 2005). "New genotype of avian influenza H5N1 viruses isolated from tree sparrows in China". Journal of Virology. 79 (24): 15460–15466. doi:10.1128/JVI.79.24.15460-15466.2005. PMC 1316012. PMID 16306617.
- ^ The World Health Organization Global Influenza Program Surveillance Network (October 2005). "Evolution of H5N1 avian influenza viruses in Asia". Emerging Infectious Diseases. 11 (10): 1515–1521. doi:10.3201/eid1110.050644. PMC 3366754. PMID 16318689. Figure 1 shows a diagramatic representation of the genetic relatedness of Asian H5N1 hemagglutinin genes from various isolates of the virus
- ^ Taubenberger JK, Morens DM (April 2010). "Influenza: the once and future pandemic". Public Health Reports. 125 (Suppl 3): 16–26. doi:10.1177/00333549101250S305. PMC 2862331. PMID 20568566.
- ^ Webster RG, Bean WJ, Gorman OT, Chambers TM, Kawaoka Y (March 1992). "Evolution and ecology of influenza A viruses". Microbiological Reviews. 56 (1): 152–179. doi:10.1128/mr.56.1.152-179.1992. PMC 372859. PMID 1579108.
- ^ "Factsheet on swine influenza in humans and pigs". European Centre for Disease Control. 2017-06-15. Retrieved 2024-06-13.
- ^ "Global AIV with Zoonotic Potential". The Food and Agriculture Organization (FAO) of the United Nations. 29 July 2020. Retrieved 2024-06-24.
- ^ Lee K, Fang J (2013). Historical Dictionary of the World Health Organization. Rowman & Littlefield. ISBN 9780810878587.
- ^ "70 years of GISRS – the Global Influenza Surveillance & Response System". World Health Organization. 19 September 2022. Retrieved 2024-06-13.
- ^ "Vaccination of poultry against highly pathogenic avian influenza – Available vaccines and vaccination strategies". efsa.europa.eu. 2023-10-10. Retrieved 2024-05-09.
- ^ "Making a Candidate Vaccine Virus (CVV) for a HPAI (Bird Flu) Virus". U.S. Centers for Disease Control and Prevention (CDC). 2024-06-03. Retrieved 2024-06-15.
- ^ "Vaccines for pandemic influenza". European Medicines Agency. Retrieved 2024-06-15.
- ^ Keown A (February 4, 2020). "FDA Approves Seqirus' Audenz as Vaccine Against Potential Flu Pandemic". BioSpace. Archived from the original on February 5, 2020. Retrieved February 5, 2020.
- ^ "Audenz". U.S. Food and Drug Administration (FDA). January 31, 2020. STN: 125692. Archived from the original on August 6, 2020. Retrieved February 5, 2020.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain.
- ^ Zheng D, Gao F, Zhao C, Ding Y, Cao Y, Yang T, et al. (2018-09-14). "Comparative effectiveness of H7N9 vaccines in healthy individuals". Human Vaccines & Immunotherapeutics. 15 (1): 80–90. doi:10.1080/21645515.2018.1515454. PMC 6363152. PMID 30148691.
- ^ "Making a Candidate Vaccine Virus (CVV) for a HPAI (Bird Flu) Virus". U.S. Centers for Disease Control and Prevention (CDC). 2024-06-03. Retrieved 2024-06-22.
- ^ a b "Zoonotic Influenza Vaccine Seqirus EPAR". European Medicines Agency (EMA). 9 October 2023. Retrieved 26 September 2024.
- ^ Poovorawan Y, Pyungporn S, Prachayangprecha S, Makkoch J (July 2013). "Global alert to avian influenza virus infection: from H5N1 to H7N9". Pathogens and Global Health. 107 (5): 217–223. doi:10.1179/2047773213Y.0000000103. PMC 4001451. PMID 23916331.
- ^ "1880-1959 Highlights in the History of Avian Influenza (Bird Flu) Timeline". Centers for Disease Control and Prevention. 2024-06-10. Retrieved 2024-07-14.
- ^ Weston P (2024-03-26). "'Cautious optimism' as penguins test positive for bird flu but show no symptoms". The Guardian. ISSN 0261-3077. Retrieved 2024-07-14.
- ^ Sencer DJ (2024). "Outbreak in Hong Kong, 1997 · Influenza: Complex Virus/Complex History · CDC Museum Digital Exhibits". CDC Museum. Retrieved 2024-07-14.
- ^ "Recommendations for Worker Protection and Use of Personal Protective Equipment (PPE) to Reduce Exposure to Highly Pathogenic Avian Influenza A H5 Viruses : Avian Influenza (Flu)". Centers for Disease Control and Prevention. Retrieved 2015-07-25.
- ^ Aditama TY, Samaan G, Kusriastuti R, Sampurno OD, Purba W, Santoso H, et al. (2012-01-04). "Avian influenza H5N1 transmission in households, Indonesia". PLOS ONE. 7 (1): e29971. Bibcode:2012PLoSO...729971A. doi:10.1371/journal.pone.0029971. PMC 3251608. PMID 22238686.
- ^ "Avian influenza A(H5N1) virus". www.who.int. Retrieved 2024-05-28.
- ^ Li FC, Choi BC, Sly T, Pak AW (June 2008). "Finding the real case-fatality rate of H5N1 avian influenza". J Epidemiol Community Health. 62 (6): 555–9. doi:10.1136/jech.2007.064030. PMID 18477756. S2CID 34200426.
- ^ a b "Factsheet on A(H7N9)". European Centre for Disease Prevention and Control. 2017-06-15. Retrieved 2024-07-15.
- ^ Li Q, Zhou L, Zhou M, Chen Z, Li F, Wu H, et al. (April 24, 2013). "Preliminary Report: Epidemiology of the Avian Influenza A (H7N9) Outbreak in China". New England Journal of Medicine. 370 (6): 520–32. doi:10.1056/NEJMoa1304617. PMC 6652192. PMID 23614499.
{{cite journal}}: CS1 maint: overridden setting (link) - ^ a b c d "Risk assessment of avian influenza A(H7N9) – eighth update". UK Health Security Agency. 8 January 2020. Retrieved 2024-07-15.
- ^ a b Liu Y, Chen Y, Yang Z, Lin Y, Fu S, Chen J, et al. (June 2024). "Evolution and Antigenic Differentiation of Avian Influenza A(H7N9) Virus, China". Emerging Infectious Diseases. 30 (6): 1218–1222. doi:10.3201/eid3006.230530. ISSN 1080-6040. PMC 11138980. PMID 38640498.
- ^ "Avian Influenza A(H7N9) virus". Food and Agricultural Organization of the United Nations. 1 June 2022. Retrieved 2024-07-15.
- ^ CDC (2024-06-03). "2010-2019 Highlights in the History of Avian Influenza (Bird Flu) Timeline". Avian Influenza (Bird Flu). Retrieved 2024-07-16.
- ^ "USGS National Wildlife Health Center – Avian Influenza Wildlife Chart". Archived from the original on 2018-02-06. Retrieved 2010-10-06.
- ^ Thacker E, Janke B (February 2008). "Swine influenza virus: zoonotic potential and vaccination strategies for the control of avian and swine influenzas". The Journal of Infectious Diseases. 197 (Suppl 1): S19–S24. doi:10.1086/524988. PMID 18269323.
- ^ Thomas P. "Bird Flu Spreads to Cattle, Raising Fears on Farms". WSJ. Archived from the original on 2024-04-04. Retrieved 2024-04-04.
- ^ Burrough E, Magstadt D, Main R (29 April 2024). "Highly Pathogenic Avian Influenza A(H5N1) Clade 2.3.4.4b Virus Infection in Domestic Dairy Cattle and Cats, United States, 2024". Emerging Infectious Diseases. 30 (7): 1335–1343. doi:10.3201/eid3007.240508. PMC 11210653. PMID 38683888. Archived from the original on 29 April 2024. Retrieved 30 April 2024.
- ^ Caserta L, Frye E, Butt S, Dimitrov K, Diel D (25 July 2024). "Spillover of highly pathogenic avian influenza H5N1 virus to dairy cattle". Nature. doi:10.1038/s41586-024-07849-4. PMC 11485258. Retrieved 27 July 2024.
- ^ Schnirring L (24 May 2024). "H5N1 avian flu viruses can persist on milking equipment surfaces". University of Minnesota. CIDRAP. Archived from the original on 23 May 2024. Retrieved 24 May 2024.
- ^ Goodman B (2024-10-08). "As bird flu outbreak expands in California, dairy farms report it's worse than they expected". CNN. Retrieved 2024-10-10.
- ^ Mellis AM (2024). "Serologic Evidence of Recent Infection with Highly Pathogenic Avian Influenza A(H5) Virus Among Dairy Workers — Michigan and Colorado, June–August 2024". MMWR. Morbidity and Mortality Weekly Report. 73. doi:10.15585/mmwr.mm7344a3. ISSN 0149-2195. PMC 11542770.
- ^ Lee CT (28 July 2017). "Outbreak of Influenza A(H7N2) Among Cats in an Animal Shelter With Cat-to-Human Transmission—New York City, 2016". academic.oup.com. Retrieved 2024-05-16.
- ^ Thiry E, Addie, Diane, Belák, Sándor, Boucraut-Baralon, Corine, Egberink, Herman, Frymus, Tadeusz, et al. (1 July 2009). "H5N1 avian influenza in cats. ABCD guidelines on prevention and management". Journal of Feline Medicine & Surgery. 11 (7): 615–618. doi:10.1016/j.jfms.2009.05.011. PMC 7128855. PMID 19481042.
- ^ Marschall J, Hartmann K (1 August 2008). "Avian influenza A H5N1 infections in cats". Journal of Feline Medicine & Surgery. 10 (4): 359–365. doi:10.1016/j.jfms.2008.03.005. PMC 10832898. PMID 18619884. S2CID 29347001.
- ^ "Avian and Pandemic Influenza: The Global Response". Avian Influenza Action Group, United States Department of State. Oct 2008.
- ^ Hameiri S (2014). "Avian influenza, 'viral sovereignty', and the politics of health security in Indonesia". The Pacific Review. 27 (3): 333–356. doi:10.1080/09512748.2014.909523. S2CID 154302060.
- ^ a b c Porter N (2012). "Risky zoographies: The limits of place in avian flu management". Environmental Humanities. 1 (1): 103–121. doi:10.1215/22011919-3609994.
- ^ a b c Alders R, Awuni JA, Bagnol B, Farrell P, de Haan N (2014). "Impact of avian influenza on village poultry production globally". EcoHealth. 11 (1): 63–72. doi:10.1007/s10393-013-0867-x. PMID 24136383. S2CID 6701416.
- ^ Porter N (2013). "Bird flu biopower: Strategies for multispecies coexistence in Viet Nam". American Ethnologist. 40 (1): 132–148. doi:10.1111/amet.12010.
- ^ a b McLeod A, Morgan N, Prakash A, Hinrichs J (2005). Economic and social impacts of avian influenza. Food and Agriculture Organisation (Report).
Further reading
[edit]- Orent W (February 20, 2006). "The Science of Avian Flu, Answers to Nine Frequently Asked Questions". Discover Magazine. Health & Medicine. pp. 59–61.
- Haugan S, Bjornson W, eds. (2009). Avian influenza: etiology, pathogenesis, and interventions. Hauppauge, NY: Nova Science Publishers. ISBN 978-1607418467.
- Seeger RM, Hagerman AD, Johnson KK, Pendell DL, Marsh TL (July 2021). "When poultry take a sick leave: Response costs for the 2014–2015 highly pathogenic avian influenza epidemic in the USA". Food Policy. 102: 102068. doi:10.1016/j.foodpol.2021.102068.
External links
[edit]World Health Organisation (WHO)
- WHO Avian influenza resource
- The United Nation's World Health Organization's Avian Flu Facts Sheet for 2006
- In-depth analysis of bird flu Symptoms & in-depth analysis on avian flu
Food and Agriculture Organization of the UN (FAO)
- FAO Avian Influenza portal Information resources, animations, videos, photos
- FAO Bird Flu disease card Archived 2005-03-16 at the Wayback Machine
World Organisation for Animal Health (OIE)
- Current status of HPAI worldwide at OIE. WAHID Interface – OIE World Animal Health Information Database
- Disease card
- Avian influenza resource By Dr. Nati Elkin – Atlases, vaccines and information.
United States
- PandemicFlu.Gov U.S. Government avian and pandemic flu information
- CIDRAP Avian Flu Overview "Avian Influenza (Bird Flu): Agricultural and Wildlife Considerations"
- US Avian Influenza Response U.S. Agency for International Development (USAID)
- Avian influenza research and recommendations National Institute for Occupational Safety and Health
- Influenza Research Database Database of influenza sequences and related information.
- Species Profile- Avian Influenza (Orthomyxoviridae Influenza Type A, subtype H5N1), National Invasive Species Information Center, United States National Agricultural Library. Lists general information and resources for Avian Influenza.
- Strategic Health Communication for Avian and Pandemic Influenza Prevention Johns Hopkins Bloomberg School of Public Health Center for Communication Programs Global Program on Avian and Pandemic Influenza.
- NIOSH Alert: Protecting Poultry Workers from Avian Influenza (Bird Flu) CDC/NIOSH recommendations for poultry workers
Europe
- European Commission Avian Influenza control measures
- Avian Influenza: Questions & Answers European Centre for Disease Prevention and Control – Official website
- FluTrop: Avian Influenza Research in Tropical Countries French Agricultural Research Center for Developing Countries (CIRAD), Avian Influenza website
